Dr. Jennifer Sheng from Johns Hopkins School of Medicine details a 2021 editorial she co-authored with Dr. Vered Stearns that was published by Oncotarget, entitled, “Innovating and expanding weight loss strategies for breast cancer survivors.”
Behind the Study is a series of transcribed videos from researchers elaborating on their oncology-focused studies published by Oncotarget. Visit the Oncotarget YouTube channel for more insights from outstanding authors.
—
Hi everyone. I’m Jenny Sheng. I’m a breast medical oncologist and an assistant professor at the Johns Hopkins School of Medicine. It’s truly a privilege to take care of patients and conduct research here at the Sydney Kimmel Comprehensive Cancer Center. At John Hopkins University, we are committed to understanding the mechanisms of cancer and new ways to treat and prevent it. Our investigators conduct research and translate all of those results directly to meet our center’s mission, which is to improve patient care. I’m excited to be here today to share some more information about the study that we recently published, as well as the editorial that I wrote with Dr. Vered Stearns.
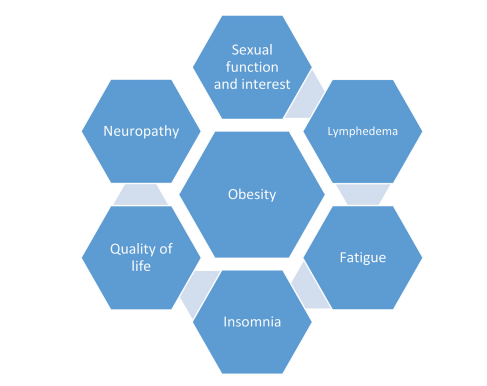
To give you a little bit of background and understand the history of the research leading up to this paper, it’s important to delve into the literature on obesity, as well as the obesity literature in breast cancer survivors. So foremost, obesity and following breast cancer diagnosis has been associated with poor quality of life and increased risk of adverse treatment effects. We know that chemotherapy can lead to weight gain. That was shown in the Well study and that loss of sexual interest, neuropathy, lymphedema, and chronic fatigue are more common in breast cancer patients who are obese compared to neuro remote weight breast cancer survivors.
In fact, weight gain may also increase the risk of recurrence by up to 50% and breast cancer related mortality by up to 60%. Thus, the NCC and the National Comprehensive Cancer Network Guidelines recommend that weight loss should be a priority for overweight or obese breast cancer survivors. And to fulfill this imperative, we have to develop successful and scalable interventions. If you’d like to read a little bit more about the history and management considerations, I’d suggest reading the editorial in oncology, which I wrote with Dr. Cesar Santa-Maria in 2018.
So as I mentioned before, our group at Johns Hopkins has been committed to the mission of delivering weight loss interventions to cancer survivors. Thus, at Hopkins, we adapted a remote intervention consisting of telephone calls by a coach, accelerometer, assess physical activity, and self-directed dietary activity monitoring. This was originally developed in the power trial and is adapted in our study and thus called the power remote trial. In this randomized clinical trial, we assessed the effects of a remote intervention versus self-directed in early stage breast cancer survivors. From 2013 to 2015, we enrolled about 96 women. At six months, we found that 50% of women randomized us to the intervention arm were able to lose at least 5% of their baseline weight. This was in comparison to only 12% of women in the self-directed arm. We also assessed changes in adipo-cytokines and metabolic factors at six months, compared to baseline.
Of note, adipo-cytokines is a general term for bioactive products produced by adipose tissue. So for instance, those include inflammatory mediators, like interleukin six or eight, angiogenic proteins, and metabolic regulators like leptin and adiponectin. In our study, we checked an array of cytokine markers. What we found to be particularly interesting is that the leptin concentration in the power remote arm was significantly decreased compared to those in the self-directed arm.
And that participants who achieved at least 5% weight loss versus those who did not had a very significant decrease in leptin. Those achieving at least 5% weight loss compared to those who didn’t actually had favorable improvements in inflammatory cytokines as well. And that includes lower interleukin one beta, CRP, and a smaller increase in MCP-1. We actually also recently published a pre-planned observational analysis of the impact of weight loss on PROs, also known as patient reported outcomes.
We had hypothesized that survivors with at least 5% weight loss would have improved physical function at six months compared to baseline. And at six months, physical function was improved in half of those with at least 5% weight loss compared to only 18% in those who did not achieve at least 5% weight loss. It’s really interesting to note that physical function was actually worse in almost a quarter of individuals with less than 5% weight loss at six months compared to just 3% in those who did achieve weight loss. While modifications in diet and exercise allow some breast cancer survivors who are overweight or obese to achieve clinically significant weight loss of at least 5%, this approach doesn’t yield similar results for all women. In fact, many studies, including ours shown that for half of women, they are not able to attain these with these type of behavioral interventions. So exploring novel domains to enhance weight loss is critical.
At present, I’m conducting a phase two study to determine whether an adaptor approach with pharmacotherapy can augment obesity treatment in breast cancer survivors. This study is called the A-NEW study, which stands for an Adaptive Nutrition and Exercise Weight Loss Study. And this is a prospective non-randomized clinical trial that assesses the effects of the addition of a pharmacotherapy, called Contrave, to a six-month behavioral weight loss intervention only in overweight or obese breast cancer patients who are unable to attain at least 5% weight loss after eight weeks of lifestyle intervention alone.
We’re also looking forward to analyzing result from the COOIN study, the Cancer, Obesity, Overweight, and Insomnia study, which was led by Dr. Janelle Coughlin. This was a randomized pilot study to better understand the relationship among insomnia, weight loss, and breast cancer. This study assesses the effectiveness of a sleep intervention prior to a web and foam based weight loss program. We look forward to sharing these results in the future.
I appreciate your time today, and I do want to acknowledge Dr. Vered Stearns, Dr. Dipali Sharma, Dr. Janelle Coughlin, Dr. Antonio Wolff, and Claire Snyder among many other colleagues at Hopkins who’ve been committed to this type of research.
TESTIMONIAL: Dr. Sheng Describes Publishing With Oncotarget
Click here to read the full research paper, published by Oncotarget.
ONCOTARGET VIDEOS: YouTube | LabTube | Oncotarget.com
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.

